Will the coronavirus we are now battling cause permanent brain damage? How many of those who recover will be affected in the future? Several key research studies have been posted this past week and the outlook is not good.
23% of recovered COVID patients have temporary brain dysfunction, 28% suffered from brain inflammation and 19% had a stroke and another 19% reported nerve damage which remains unresolved
There are now detailed reports of brain illnesses emerging from people who have been COVID positive but with relatively mild lung afflictions. We are still learning about this virus but scientists and doctors agree that it can select and choose which organs and systems it affects and it is not the same in every individual. This makes a unilateral therapeutic approach almost impossible. A drug or treatment which works for one person may not make any difference in another leaving physicians frustrated.
One key thing that we are seeing is that severe lung or cardiac complications don’t necessarily correlate with the severity of neurological illness. Having a mild case of COVID-19 respiratory complications does not mean that the individual won’t show a wide array of brain inflammation or blood clots all over the body.
Experts at the University College London (UCL) were the latest to describe that Covid-19 could cause neurological complications including stroke, nerve damage, and potentially fatal brain inflammation — even if the patients didn’t show severe respiratory symptoms associated with the disease.
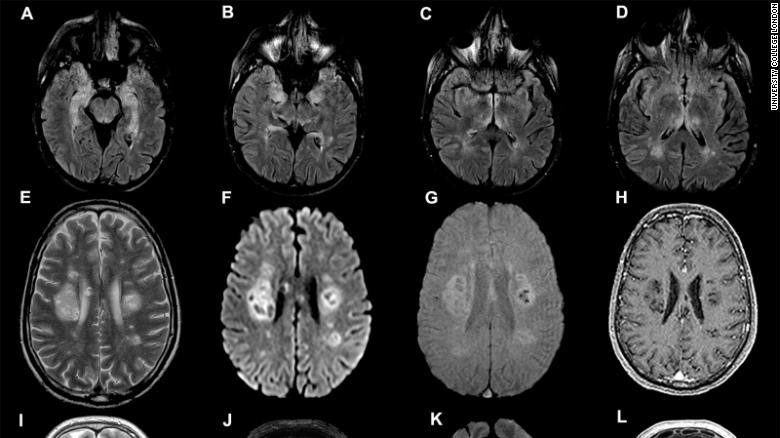
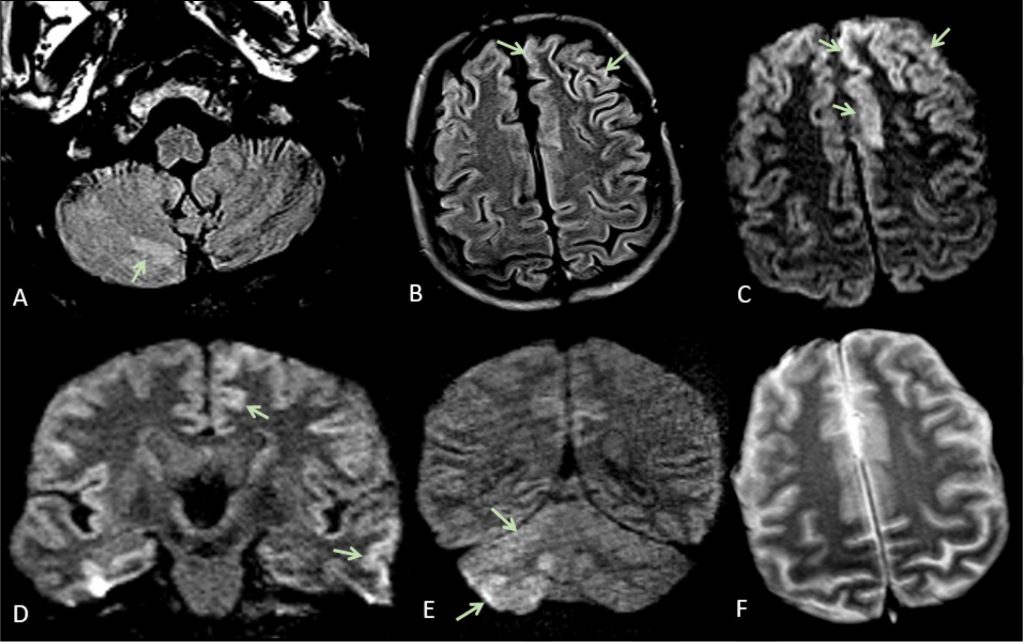
The study, published in the journal Brain, examined 43 patients treated at University College London Hospitals for either confirmed or suspected coronavirus, from April to May. They varied in age from 16 to 85, and showed a range of mild to severe symptoms. Among these patients, researchers found 10 cases of “temporary brain dysfunction” and delirium; 12 cases of brain inflammation; eight cases of strokes; and eight cases of nerve damage
“We should be vigilant and look out for these neurological complications in people who have had Covid-19” Dr. Michael Zandi.
Most of the patients who showed brain inflammation were diagnosed with a specific, rare and sometimes deadly condition known as Acute disseminated encephalomyelitis (ADEM).
Before the pandemic, the research team in London would see about one ADEM patient per month. During the study period, the number rose to at least one a week.
One woman hallucinated lions and monkeys in her house. Others reported numbness in their limbs or face, double vision, and disorientation. One severe patient was barely conscious, responding only when in pain.
Researchers are still trying to figure out why exactly Covid-19 patients are developing these brain complications. The virus that causes Covid-19 was not found in their brain fluid, meaning the virus does not appear to directly attack the brain. One theory, instead, is that the complications are indirectly triggered by an immune response from the patient’s body — not from the virus itself.
These findings are significant for informing how doctors around the world monitor and treat patients — but they also pose new questions and challenges. For patients who aren’t showing severe respiratory symptoms such as trouble with breathing, it can be difficult to identify these brain complications early enough to prevent or minimize damage. And for patients who are critically ill, their precarious health can limit how much doctors can do to investigate what’s happening in their brain. The authors warned that further studies will be “essential” in figuring out how exactly the virus causes brain damage, and how to treat it.
“Given that the disease has only been around for a matter of months, we might not yet know what long-term damage Covid-19 can cause,” Dr. Ross Paterson
We’ve already seen that some people with Covid-19 may need a long rehabilitation period — both physical rehabilitation such as exercise, and brain rehabilitation. We need to understand more about the impact of this infection on the brain. These neurological complications seem to be taking one of 4 different forms:

- A confused state (known as delirium or encephalopathy), sometimes with psychosis and memory disturbance.
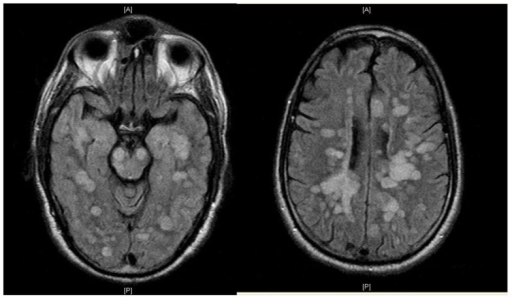
- Inflammation of the brain (known as encephalitis). This includes a form showing inflammatory lesions – acute disseminated encephalomyelitis (ADEM) – together with the effects of low oxygen in the brain.
- Blood clots, leading to stroke (including in younger patients).
- Potential damage to the nerves in the body, causing pain and numbness (for example in the form of post-infectious Guillain-Barré syndrome, in which your body’s immune system attacks your nerves).
The virus also has the potential to infect the brain directly. However, most of the physical effects we’ve seen in survivors look like the secondary impacts of the virus being present in the brain rather than the effects of direct infection. For example, our immune system can appropriately fight the virus, but may start to attack our own cells – including our brain cells and nerves. This may be through the actions of immune cells and antibodies via an inflammatory mechanism known as a cytokine storm, or through mechanisms we don’t yet understand.
There are also Covid-19 patients having ischaemic strokes, where a blood clot blocks the flow of blood and oxygen to the brain. Some of these patients have stroke risk factors (for example high blood pressure, diabetes or obesity), though their strokes have been particularly severe. It seems that this is because the blood rapidly becomes thickened in Covid-19 and, in these patients, there have been multiple blood clots in the arteries feeding blood to the brain, even in patients already receiving blood thinners. In others, there is brain bleeding due to weakened blood vessels, perhaps inflamed by the effects of the virus.
Where infection with the coronavirus is associated with inflammation or damage to the nerve endings themselves, individuals may develop burning and numbness and also weakness and paralysis. Often it’s difficult to know if these are the effects of critical illness on the nerves themselves or if there are additional aspects of brain and spine involvement.
All of these effects on the brain and nervous system have the potential for long-term damage and can stack up in an individual. But we need to know more about what’s going on in people’s nervous systems before we can accurately predict any long-term effects.
One way of finding out more is to take a look inside patients’ heads using brain-imaging techniques, such as MRI. So far, brain imaging has revealed a pattern of previously unseen findings, but its still very early days for using it in this pandemic.
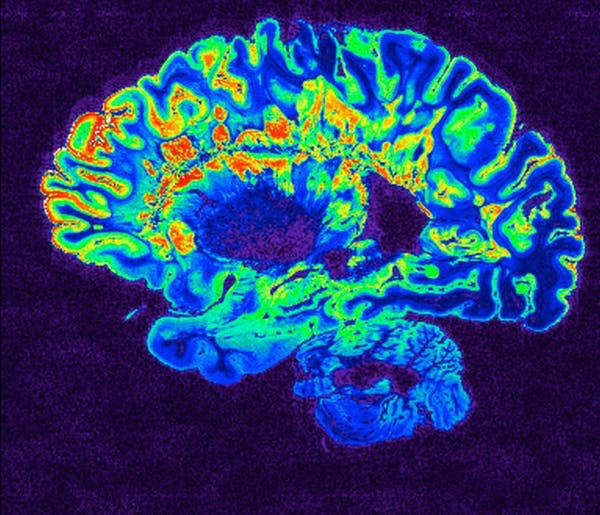
In one study, patterns found included signs of inflammation and a shower of small spots of bleeding, often in the deepest parts of the brain. Some of these findings are similar to those seen in divers or in altitude sickness. They might represent the profound lack of oxygen being delivered to the brain in some patients with Covid-19 – but we are only starting to understand the full scope of the brain’s involvement in the disease. Brain-imaging and postmortem studies for those killed by Covid-19 have been limited to date.
The main thing that all of the studies have in common is how humbling they are and how they illustrate how much we still do not know about this virus.